Cardiomyopathy and Blood Pressure – How Are They Linked?
Health hazards such as high blood pressure and heart failure are well-known among the general population. But cardiomyopathy?
Not so much. It doesn’t help that the term is a bit of a mouthful. Thanks, scientists. If you or somebody close to you has received a diagnosis of this disease – or you’re hearing of it for the first time – you’ll no doubt have lots of questions.
What are the causes? Is it reversible? And what’s the link between cardiomyopathy and blood pressure?
Let’s get those queries answered for you in today’s easy-read guide.
What is cardiomyopathy?
Cardiomyopathy doesn’t refer to one specific condition. Instead, it’s an umbrella term for a group of diseases that cause the walls of the heart chambers to become abnormal – enlarged, thickened, weaker, or stiff.
You might think that a larger, thicker heart would be stronger and more robust to help you live a long life. Alas, that’s not how it works in reality. Changes to the size or structure of your heart can both:
- Limit its ability to pump blood around the body efficiently, and
- Interfere with its ability to process electrical signals, leading to heartbeat abnormalities
How many different types of cardiomyopathy are there?
We’ll begin by explaining the three most common types of cardiomyopathy to be aware of:
- Hypertensive cardiomyopathy
Caused by long-standing high blood pressure, hypertensive cardiomyopathy is a specific form of heart muscle disease. When blood pressure is high, this makes the heart have to work harder to pump blood around the body. What happens over time?
The heart muscle becomes thicker and stiffer, which results in hypertensive cardiomyopathy.
The health impact of this disease is significant. Hypertensive heart disease accounts for most cases of heart failure in adults between the ages of 25 and 69. Such statistics are a sober reminder for people with hypertension to do all they can to reduce their blood pressure (or at least stop it from rising further).
Important facts to be aware of:
- Hypertensive cardiomyopathy can stop the heart from being able to fully relax between beats. This leads to reduced blood flow.
- Women are more at risk of developing hypertensive cardiomyopathy following hormonal changes during menopause.
- There are asymptomatic cases of hypertensive cardiomyopathy. So, it’s wise to get regular heart check-ups with your doctor.
- Hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy (HCM) is the most common genetic heart disease. Like in hypertensive cardiomyopathy, it causes the heart muscle to become thicker and stiffer. This is double-trouble for the cardiac system. Reason being?
The filling capacity of the heart reduces, which restricts the amount of blood it can pump around the body with each beat. Thickened heart walls may also disturb how well it can receive electrical signals. This change in function can produce an abnormal heart rhythm (arrhythmia) and a greater risk of cardiac arrest.
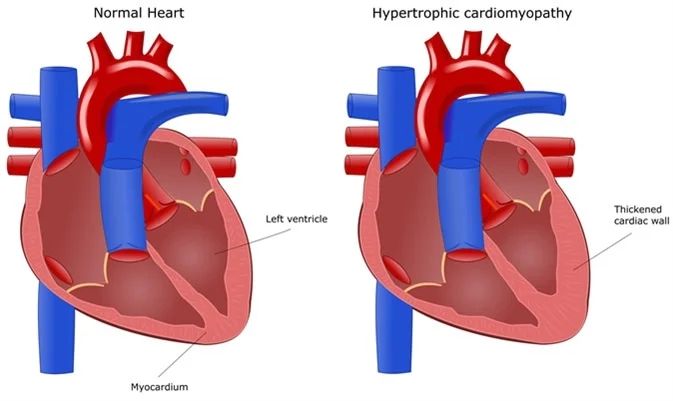
A representation of a normal heart vs. a heart with hypertrophic cardiomyopathy. Note the thickened cardiac wall in the lower chambers of the heart. Image source: News Medical
Important facts to be aware of:
- Around 1 in 500 adults have HCM.
- A child born to a parent with HCM has a 50% risk of developing it too.
- HCM is known to be a leading cause of sudden cardiac death in young people.
- Dilated cardiomyopathy
In dilated cardiomyopathy (DCM), the lower chambers of the heart become larger and weaker.
This effect both stretches and thins the heart muscle walls. As a result, the ventricles of the heart may no longer be able to pump blood around the body at the right pressure.
Important facts to be aware of:
- DCM is most common in adults under the age of 50.
- Aside from genetics, the top risk factors for DCM include diabetes, high blood pressure, and viral infection.
- Previous research highlights a five-year mortality rate of around 50% and a one-year mortality rate of 25-30% for those with DCM.
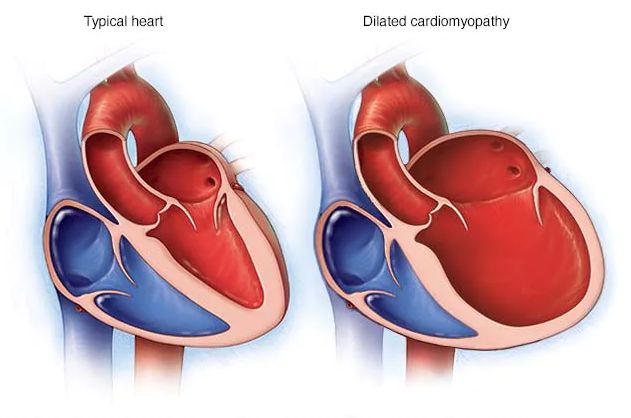
A representation of a typical heart vs. a heart with dilated cardiomyopathy. Note the enlarged lower chamber of the heart with thinner muscle walls. Image source: Mayo Clinic
As well as cardiomyopathy due to hypertension, there are several rarer types. Here is a quick overview:
- Arrhythmogenic cardiomyopathy
An inherited heart disorder. The proteins that bind the heart’s muscle cells are abnormal, often leading to heart rhythm issues and predisposition to sudden cardiac death in young people.
- Left ventricular noncompaction
In this disorder, the lower left ventricle is atypical. Instead of being smooth and firm, it is thicker and spongier, which affects its ability to pump blood around the body.
- Restrictive cardiomyopathy
A rare form of cardiomyopathy. The heart is not able to fill with blood as the chambers cannot relax as they should after contracting. It’s seen most commonly in children.
- Takotsubo cardiomyopathy
Also called “broken heart syndrome,” this can occur after acute stress such as bereavement or surgery. While the heart shows no signs of coronary heart disease, there is a sudden weakening of the left ventricle. It may mimic the symptoms of a heart attack.
The symptoms of cardiomyopathy vs. the symptoms of high blood pressure
Cardiomyopathy isn’t always easy to identify in the early stages, as the symptoms can be subtle. They become more prominent as the condition advances.
Here is a list of common symptoms to watch out for:
- Abnormal heartbeats or murmurs
- Chest pain (especially after eating or physical activity)
- Dizziness, lightheadedness, or fainting
- Increased fatigue
- Shortness of breath (especially after exertion)
- Swelling in the abdomen, feet, or legs
Dizziness. Shortness of breath. Notice how many of these are also common symptoms of high blood pressure?
It’s no surprise when you consider that cardiomyopathy and hypertension are both disorders of the cardiac system that put an added strain on the heart.
Get exclusive access to our expert insights and tips for accurate blood pressure monitoring. Sign up for our newsletter today!
What’s the link between cardiomyopathy and blood pressure?
Inherited genetic mutations are the primary cause of most types of cardiomyopathy. Even so, there is a clear connection between cardiomyopathy and blood pressure in many cases.
- High blood pressure (hypertension) left untreated can develop into cardiomyopathy
- Cardiomyopathy often leads to heart failure
- Heart failure increases the risk of cardiac-related death
To highlight an example at the individual level, a series of health events could look like this:
A 50-year-old man has long-term high blood pressure (hypertension). After five years of untreated hypertension, he develops cardiomyopathy. After another couple of years, he experiences heart failure. He passes away five years later from a cardiac arrest at age 62.
People with long-term high blood pressure have narrower, less supple arteries. Blood is not able to move throughout the body as easily, which makes the heart work harder.
Over time, the extra workload can affect the structure of the heart chambers and muscle walls. It can stop them from being able to pump enough blood to maintain full cardiac functions.
Can cardiomyopathy be treated?
While cardiomyopathy can’t be cured, there are many effective treatments to help control and lessen the impact of symptoms. For those with inherited cardiomyopathy, The British Heart Foundation states that “in most cases living with it will not affect your quality or length of life.”
Treatment will depend on the type of cardiomyopathy and other conditions or co-morbidities. Options may include:
- Medication: Anticoagulants, beta-blockers, and diuretics are among those often offered to patients.
- Pacemaker/Defibrillators: A small device is inserted in the chest to regulate heartbeat rhythms via electrical impulses or treat dangerous heart rhythms.
- Cardioversion: Electrode pads connected to a defibrillator are placed on the chest to send electric signals. These restore normal heart rhythm.
- Ablation: Either heat or freezing is used to remove damaged areas of the heart that cause abnormal rhythms.
- Heart surgery (or heart transplant): This is only likely to be recommended if other treatments above have failed.
Your doctor may also recommend a series of lifestyle changes, such as:
- Controlling blood pressure and blood sugar levels
- Getting regular exercise
- Limiting alcohol intake
- Lowering cholesterol by swapping saturated for unsaturated fats
- Maintaining a healthy weight
- Quitting smoking
- Reducing stress
Please make sure to consult with your doctor about any potential treatments.
Monitoring Your Blood Pressure With Aktiia
Uncontrolled high blood pressure is one of the key risk factors for non-genetic cardiomyopathy. If you or a loved one has hypertension, it’s vital to have a reliable way of measuring blood pressure to make sure it doesn’t spiral out of control.
Aktiia allows you to do just that. Worn around the wrist, the Aktiia monitor provides 24/7 blood pressure tracking with automatic measurements day and night.
Aktiia helps people with high blood pressure to track their cardiac health.
If you wish, you can go here to view customer reviews and see the full benefits of Aktiia.
Thanks for stopping by today. We hope the article has been helpful.
Team Aktiia
Disclaimer: If you are concerned about your blood pressure, it is best to speak to your doctor. They can advise on the best way to manage your blood pressure.
Sources:
Hypertrophic Cardiomyopathy (HCM). News Medical Life Sciences. December 2022 – https://www.news-medical.net/health-hypertrophic-cardiomyopathy
Stable Rates of Obstructive Hypertrophic Cardiomyopathy in a Contemporary Era. Frontiers in Cardiovascular Medicine. January 2022 – https://www.ncbi.nlm.nih.gov/articles-PMC8770922
Dilated cardiomyopathy. Mayo Clinic. May 2022 – https://www.mayoclinic.org/diseases-dilated-cardiomyopathy-symptoms-causes
Fifteen-year mortality and prognostic factors in patients with dilated cardiomyopathy: persistent standardized application of drug therapy and strengthened management may bring about encouraging change in an aging society. Journal of Geriatric Cardiology. May 2022 – https://www.ncbi.nlm.nih.gov/articles-PMC9170907
Cardiomyopathy. NHS. November 2019 – https://www.nhs.uk/conditions-cardiomyopathy
Symptoms and Diagnosis of Cardiomyopathy. Heart.org. May 2022 – https://www.heart.org/en/health-cardiomyopathy-symptoms-and-diagnosis-of-cardiomyopathy